

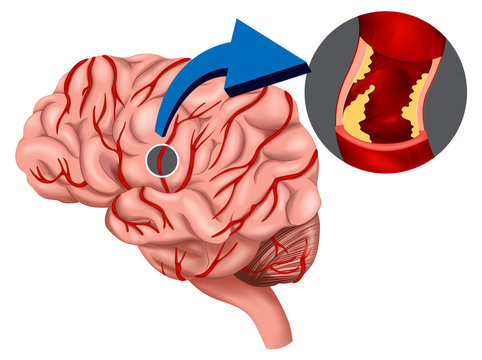
Subdural hematoma (SDH) is a serious condition characterized by the accumulation of blood between the layers of the dura mater and arachnoid membrane surrounding the brain. It typically occurs as a result of trauma, often due to head injuries or sudden acceleration/deceleration forces that cause blood vessels to tear and bleed. SDH can range from mild to life-threatening, depending on the extent and rate of bleeding.
SDH most commonly results from traumatic brain injury (TBI), such as falls, motor vehicle accidents, assaults, or sports injuries, where the brain shifts rapidly within the skull. This movement can cause blood vessels, especially bridging veins that connect the brain's surface to deeper venous structures, to stretch or tear, leading to bleeding. In elderly individuals, SDH can sometimes occur spontaneously due to minor trauma or underlying brain atrophy.
Symptoms of SDH can develop immediately after trauma or appear gradually over hours to days, depending on the size and rate of bleeding. Common symptoms include:
Often severe and persistent.
Disorientation or altered mental status.
Especially if accompanied by increased intracranial pressure.
Certain genetic factors can predispose individuals to develop osteoarthritis.
Ranging from drowsiness to coma in severe cases.
Diagnosis of SDH involves a combination of clinical assessment, imaging studies, and sometimes invasive procedures:
The most common initial imaging study to detect and assess the size and location of the hematoma.
Sometimes used for further evaluation, especially if a chronic SDH is suspected.
Including neurological examination to assess cognitive function, motor strength, and reflexes.
Treatment of SDH depends on its severity, size, and the patient's clinical status:
Small, asymptomatic SDH may be managed conservatively with close monitoring and repeated imaging to ensure stability.
Large or symptomatic SDH often requires surgical intervention to evacuate the hematoma and relieve pressure on the brain. This may involve craniotomy (opening the skull) or less invasive techniques such as burr hole evacuation.
Medications may be administered to control seizures, manage pain, or prevent complications such as brain swelling.
The prognosis for SDH varies widely depending on factors such as age, overall health, size of the hematoma, and timeliness of treatment. Prompt diagnosis and appropriate management are crucial for minimizing neurological deficits and improving outcomes. Complications can include permanent neurological damage, recurrent bleeding, or infection.